- EEG
- Ambulatory EEG
- VEEG
- VNS
- RNS- Responsive Neurostimulation
- Epilepsy Surgery
- Epilepsy Monitoring Unit
- LITT
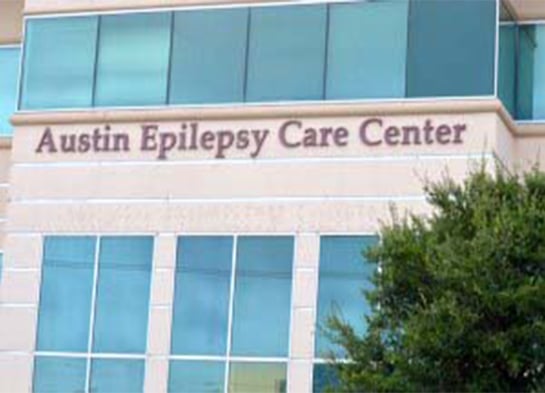
Electroencephalography (EEG)
An electroencephalogram (EEG) is a diagnostic test that measures the electrical activity of the brain in order to detect and evaluate neurological conditions such as epilepsy, dementia, as well to determine the rate of recovery for patients who are unconscious or in a coma.
During the EEG procedure, electrodes are placed on the head to record the electrical activity in the brain, which is interpreted by the doctor. Patients will be asked to breath deeply, look at bright, flashing lights or go to sleep in order for the doctor to collect a range of brain activity. Brain activity is produced as a series of wavy lines that are analyzed by the doctor.
There is no pain associated with the EEG procedure.
Ambulatory Electroencephalogram (EEG)
An ambulatory electroencephalogram, or EEG, is a neurodiagnostic test that measures and records the brain's electrical activity using a small, portable monitor. It can record up to 72 hours of the brain's electrical activity, and the test is conducted as the patient goes about their normal activities. Ambulatory EEG is commonly used to diagnose epilepsy.
The electrodes are placed on the patient's scalp. These electrodes are connected by wires to the portable monitor that records the brain's electrical activity. Patients are given instructions to follow during the test, which may take more than a day to complete. While ambulatory EEG is considered a safe, painless procedure, some patients experience temporary skin irritation in areas that had come into contact with the electrodes. The results of an ambulatory EEG are interpreted by a neurologist.
Video EEG Monitoring
Video-EEG monitoring is done at the Epilepsy Monitoring Unit (EMU) in the Hospital. The epilepsy monitoring unit is the gold standard in the diagnosis and management of epilepsy. This type of monitoring allows the epileptologist to determine the type of epilepsy the patient has and the best long term treatment options.
It also helps to determine whether the individual's events or symptoms are related to seizures. Video EEG monitoring consists of simultaneous video and EEG recording. The video monitoring is used to observe the clinical and behavioral changes of the individual during a seizure or an event. Simultaneous EEG monitoring will help localize the area in the brain that is involved at the onset of the seizure.
This is a crucial test prior to considering epilepsy surgery.
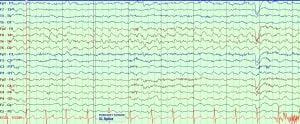
Vagus Nerve Stimulation
Vagus nerve stimulation is a therapeutic treatment that sends electric signals to the brain through a small device that is implanted underneath the skin of the chest. This device, known as as a vagus nerve stimulator, sends pulses of electrical energy to the vagus nerve and to the brain, which helps to inhibit seizures in many patients with epilepsy.
The vagus nerve is one of twelve cranial nerves in the brain, and it sends messages from the brain to the body's major organs including the heart, lungs and intestines, and to areas of the brain that control mood, sleep, and other functions. Research has indicated that when stimulated by electrical impulses, the vagus nerve sends messages to the brain that help to stop seizures from occurring, and may also help to control mood in people suffering from depression.
Responsive Neurostimulation
The Responsive Neurostimulation System, or RNS®, is an FDA-approved device, designed to control and reduce the frequency of epileptic seizures in adults. RNS may be recommended for patients who suffer from frequent seizures. Good candidates typically include individuals whose epilepsy cannot be controlled by medications and those ineligible for epilepsy surgery, which usually involves removing part of the brain to reduce seizure activity.
RNS devices are surgically implanted into the skull by a neurosurgeon, and are powered by a battery with advanced technology that can record the brain's electrical activity. When the device detects abnormal electrical activity in the brain, it delivers small amounts of electrical currents to curb the seizure activity. The battery within the device requires replacement after about three years.

While not a cure for epilepsy, RNS is effective for reducing the frequency and severity of epileptic seizures.
Epilepsy Surgery
Epilepsy is a neurological disorder caused by disturbances in brain activity that result in recurrent seizures. Although seizures may be mild, all forms of epilepsy should be treated, as seizures may put individuals in danger during certain activities. While medications are often effective in preventing seizures, some cases of epilepsy do not respond to anti-seizure drugs and may require surgery.
The most common method of epilepsy surgery is removing the area of the brain where the seizures originate to reduce or eliminate seizure activity. Potential risks of epilepsy surgery include memory problems, impaired vision, infection, bleeding, and language difficulties. Results of epilepsy surgery vary, but many patients who are good candidates for surgery become completely seizure-free. Use of anti-seizure medications should continue for at least 1-2 years after surgery.
Thermal Ablation Therapy, LITT:
Laser Interstitial Thermal Ablation, LITT is a minimally invasive technique to ablate the seizure focus and stop recurrent seizures. It is considered when there is only one seizure focus, typically mesial temporal seizure focus or hypothalamic hamartoma, or deep brain lesions. Epileptologists and neurosurgeons will review the pre-surgical tests and determine if LITT is an appropriate treatment to consider vs. open craniotomy (traditional brain epilepsy surgery).
LITT uses laser to cause directed and controlled heat in specific area in the brain to remove the seizure focus. For appropriate cases, the procedure is done under general anesthesia, but shorter in duration compared to traditional craniotomy. MRI of brain will be taken prior to the procedure for surgical planning and then more MRI images are taken during the procedure to monitor the thermal ablation.
The patient will stay in the hospital for 1-2 days and then goes home. The recovery time is shorter than traditional surgery. Most side effects are headaches, rarely bleed or infection.